e-News
Teaching Development Grants (TDG)
Teaching Development Grants (TDG)
 |
“Students as Partners” in Promoting Healthy Aging: Using Online Co-Teaching to Enhance Nursing Students’ Clinical ReasoningPrincipal Investigator: Dr Maggie Mee Kie Chan, School of Nursing
|

|
Exploring Photo-elicitation as a Teaching & Learning Tool to Foster Medical Student’s Awareness of Age-related Biases in Healthcare and to Develop a Humanist View of AgeingPrincipal Investigator: Mr Samson Ki Sum Wong, Medical Ethics and Humanities Unit
|
 |
The Adopting of an Interactive Hybrid Teaching Mode to Promote Undergraduate Nursing Students’ Clinical ReasoningPrincipal Investigator: Dr Veronica Suk Fan Lam, School of Nursing
|
 |
Leveraging the Pandemic as to Accelerate Holistic Telemedicine Curriculum Development in Hong Kong – Covering Patient Management Lifecycle from Consultation to Investigation and TreatmentPrincipal Investigator: Dr Siu Han Jo Jo Hai, Department of Medicine
|
 |
From Literacy to Actual Collaboration: Applying a Spiral Approach to a Large-scale Cross-Faculty Interprofessional Education and Collaborative Practice Model for HKUPrincipal Investigator: Fraide Jr. Agustin Ganotice, Bau Institute of Medical and Health Scie
|
 |
Professional Skills in Communication and Prioritization in Acute CarePrincipal Investigator: Dr Abraham Ka Chung Wai, Emergency Medicine Unit
|
 |
Scaffolding Clinical Teaching by Video-based Interactive Modules (VIMs) Through DIY Video Recording of Clinical EncountersePrincipal Investigator: Dr Gordon Tin Chun Wong, Department of Anaesthesiology
|
 |
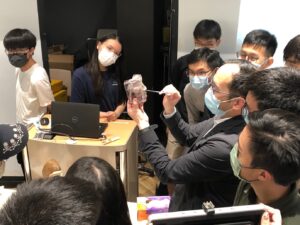
Advanced 3D Printed Models for Multidisciplinary Undergraduate Clinical Teaching”Principal Investigator: Tak Man Wong, Department of Orthopaedics & Traumatology
|
 |
1. New Capstone Experience in Undergraduate-initiated Biomedical Research with Interdisciplinary Collaboration and Student-patient InteractionsPrincipal Investigator: Dr Joseph Yau Kei Chan, Department of Ophthalmology
|
 |
1. Interprofessional Interactive Learning Module on Inhaler Devices for the Management of Respiratory Disorders – A Student Partnership ApproachPrincipal Investigator: Dr Esther Wai Yin Chan, Department of Pharmacology & Pharmacy
|
 |
A Living Library of Patient-Educators for Virtual Teaching, Learning and Assessment of Clinical Consultation Skills for Medical StudentsPrincipal Investigator: Dr Esther Yee Tak Yu, Department of Family Med & Primary Care
|
 |
Construction of a Pharmaceutical Chemical Virtual Laboratory to Facilitate Inquiry-based Learning in the Pharmaceutical Chemical Education of the BPharm ProgrammePrincipal Investigator: Dr Kong Ching Wong, Department of Pharmacology & Pharmacy
|
 |
Teaching Data Science Skills in Biomedical Sciences and Medical CurriculaPrincipal Investigator: Dr Joshua Wing Kei Ho, School of Biomedical Sciences
|